Tyrone Burke, October 28, 2020
Decontaminating N95 masks could help address personal protective equipment shortages during the second wave of the pandemic
As though the spectre of a deadly disease quietly spreading through our communities wasn’t enough, a widespread shortage of masks, gloves and face shields added uncertainty to the early days of the COVID-19 pandemic.
“We weren’t sure if we were going to have enough N95 masks to protect our health care workers, if there was a huge flood of coronavirus cases,” says Alex Wong, an Associate Professor in the Department of Biology.
“We didn’t have a big enough stockpile, and the whole world was asking for N95 masks at the exact same time.”
During the spring of 2020, Canadians flattened the curve, and that helped reduce the need for PPE. But the second wave of COVID-19 has already arrived, and this time around we are less likely to see the kind of blanket lockdowns that ground the country to a virtual halt. As cases of COVID-19 rise, the demand for PPE could be higher than ever.
Canada’s manufacturing sector has increased domestic production of PPE, and we are no longer as reliant on foreign companies for PPE as we were in early 2020. But decontaminating PPE so that it can be re-used could also help meet increased demand.
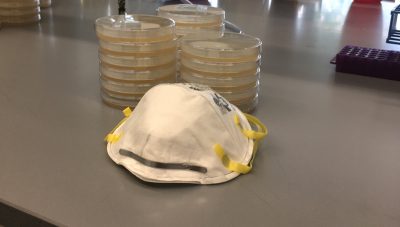
Through a NSERC Alliance Grant, Wong is teaming up Ottawa-based custom LED light manufacturer Arkalumen and the Children’s Hospital of Eastern Ontario (CHEO) to create a, ultraviolet (UV) light decontamination cabinet for N95 masks. The unit resembles a mini fridge, and used N95 masks are attached to its door for a period of decontamination.
“We are doing a series of experiments to figure out how much UV-C light is needed to kill different kinds of pathogens,” says Wong.
“We have been experimenting with the wavelength and dose that are needed to kill different bacteria and pathogens. It’s coming along, and is looking pretty promising.”
This decontamination technology could have applications that extend far beyond COVID-19 pandemic. It could help us manage future pandemics, and deliver better medical care in remote or hard to reach locations.
“Any pathogen that we run into should be susceptible to UV decontamination. It’s just a matter of how much,” says Wong.
“The decontamination unit could be used in remote locations. For example, by the Red Cross during a humanitarian emergency, or at a military field hospital. It could be taken in to the field to decontaminate PPE, if it is in short supply. It could have all sorts of all sorts of applications.”
Share: Twitter, Facebook
